.png)
The 2026 Medicare Physician Fee Schedule (PFS) includes targeted reimbursement updates for cardiac implantable electronic device (CIED) remote monitoring, most notably a substantial increase in payment for the technical component that supports remote device interrogation.
The changes do not alter clinical indications for remote monitoring, nor do they meaningfully expand the scope of covered services. Instead, they recalibrate payment to better reflect the operational and technical infrastructure required to support remote monitoring at scale.
For cardiology and electrophysiology practices, the update reinforces remote monitoring as a long-term, embedded component of cardiovascular care, while shifting attention toward execution, workflow reliability, and operational maturity.
What Changed in the 2026 Physician Fee Schedule
CMS updated reimbursement for CPT codes 93294–93298, which cover professional and technical services associated with remote interrogation and monitoring of pacemakers, ICDs, implantable loop recorders, and implantable physiologic monitors.
The most consequential change is the revaluation of CPT 93296, the technical component of remote device interrogation.
Key elements of the update include:
- An approximately 63% increase in reimbursement for CPT 93296
- Modest increases (generally 4–6%) across other CIED remote monitoring codes
- A small reduction in physician work RVUs (approximately 1.7–2.7%) applied broadly across non–time-based services
In aggregate, total reimbursement for CIED remote monitoring increases, with a greater share attributed to practice expense rather than physician work.
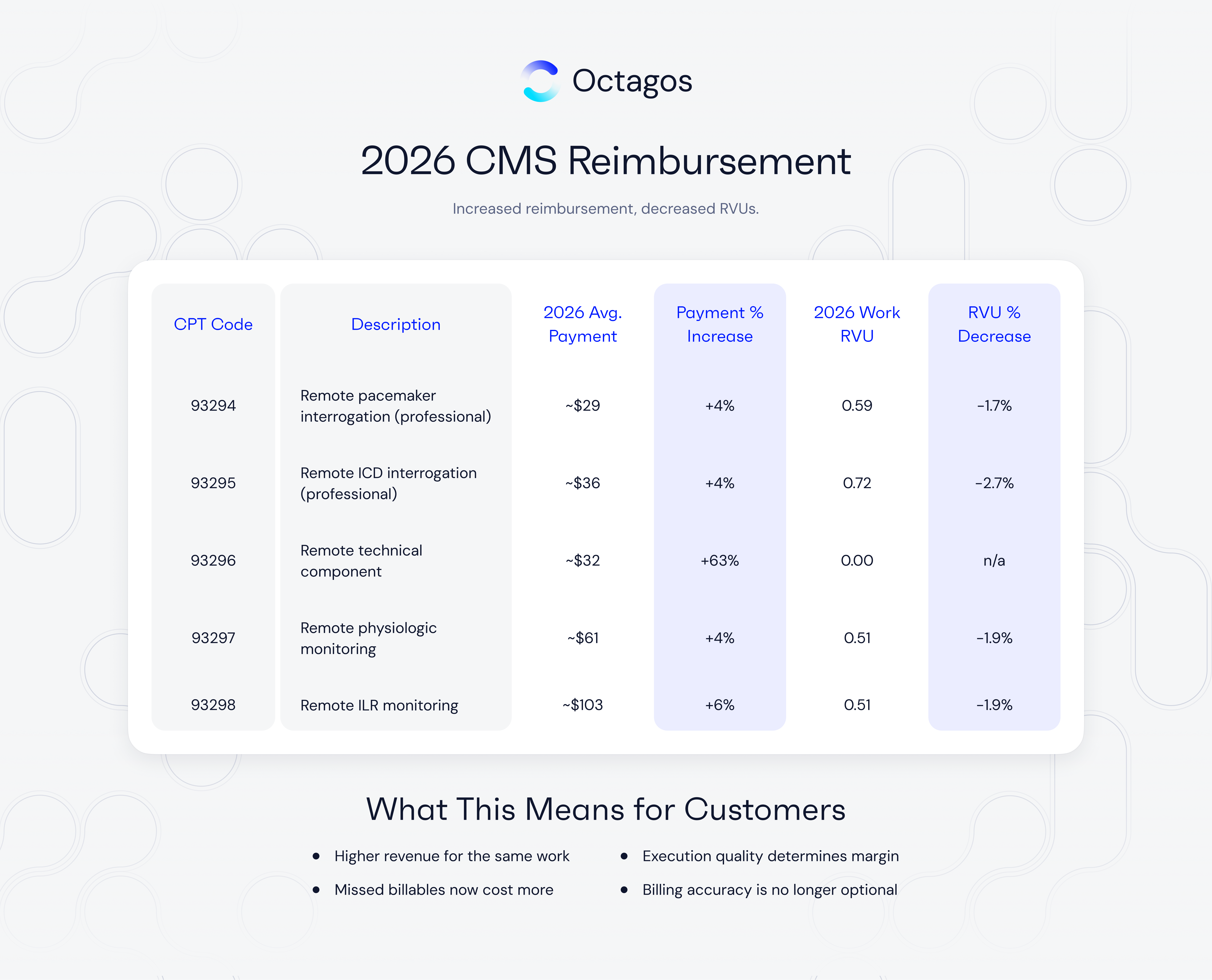
Note: For simplicity, professional and technical components are shown in aggregate; CMS pricing includes modifier-specific variation.
Figures reflect national averages; geographic adjustments apply. RVU changes are consistent with CMS’s 2026 efficiency adjustment applied to non–time-based services.
Why CMS Revalued CPT 93296
CPT 93296 supports the technical infrastructure required for remote device monitoring. It encompasses the non-physician labor and systems required to receive, process, normalize, and prepare device data for clinical review.
Operationally, the technical component includes:
- Data ingestion across multiple device manufacturers
- Staff time for triage, normalization, and queue management
- Patient connectivity monitoring and troubleshooting
- Secure systems for data handling, storage, and documentation
Prior reimbursement levels did not fully account for the complexity or scale of this work. As device populations expanded and monitoring expectations increased, many clinics experienced staffing strain, delayed workflows, and operational inefficiencies.
By updating practice expense assumptions and staffing models, CMS acknowledged that remote monitoring is resource-intensive and dependent on sustained technical and operational investment.
Interpreting the Work RVU Adjustment
CMS applied a modest efficiency adjustment to physician work RVUs across many non–time-based services, including CIED remote monitoring.
In practical terms:
- Physician RVU credit per service is slightly reduced
- Total reimbursement remains stable or increases
- The adjustment does not signal reduced clinical importance
For most practices, the RVU change is incremental and outweighed by improved reimbursement for the technical infrastructure that supports the service.
Implications for Cardiology and EP Practices
Improved Financial Sustainability
The 2026 update materially improves the financial viability of remote monitoring programs, particularly for practices managing large device populations. Practices are better positioned to maintain staffing levels, support consistent follow-up cadence, and reduce reliance on deferred monitoring.
Increased Visibility into Operational Performance
As reimbursement improves, operational variability becomes more consequential. Missed transmissions, delayed reviews, and incomplete documentation now represent not only clinical gaps but measurable revenue leakage.
High-functioning programs increasingly demonstrate:
- Consistent patient transmission compliance
- Predictable review intervals
- Documentation aligned with CMS billing frequency requirements
Reinforcement of Remote Monitoring as Baseline Care
CMS’s continued investment reinforces remote monitoring as an expected standard rather than an optional adjunct. Operational limitations, rather than reimbursement, increasingly define program performance.
Persistent Operational Constraints
Despite improved reimbursement, many device clinics continue to face:
- Alert fatigue and staff overload
- Fragmented workflows across device manufacturers
- Manual processes that scale poorly with volume
- Inconsistent patient engagement and connectivity
These challenges are largely operational in nature and are not resolved by reimbursement adjustments alone.
Care Models Aligned with CMS Policy Direction
The 2026 updates implicitly favor care models that:
- Standardize workflows across device types
- Reduce non-actionable data burden
- Improve reliability of patient connectivity
- Support consistent documentation and billing
Some practices address these requirements internally, while others rely on integrated platforms or external operational support. Solutions such as Octagos are designed to support these objectives by consolidating workflow, data infrastructure, and clinical support functions. Regardless of delivery model, execution discipline is increasingly the determinant of program success.
Questions Practices Should Be Asking in 2026
- Are all eligible patients transmitting on schedule?
- Are review and documentation workflows consistent and scalable?
- Are billable events reliably captured within CMS frequency rules?
- Can current systems support growth without increasing burnout?
The answers to these questions increasingly determine whether reimbursement improvements translate into improved care delivery.
Outlook
The 2026 CMS updates represent a course correction rather than a strategic shift. CIED remote monitoring remains clinically essential, and reimbursement has been adjusted to better reflect the operational realities required to deliver it effectively.
For practices, the constraint is no longer reimbursement alone.
It is operational execution.